
INTEGUMENTARY SYSTEM NURSING ASSESSMENT NCLEX Review YouTube
14.6 Checklist for Integumentary Assessment Use this checklist to review the steps for completion of an "Integumentary Assessment." Steps. Disclaimer: Always review and follow agency policy regarding this specific skill. Gather supplies: penlight, nonsterile gloves, magnifying glass (optional), and wound measuring tool (optional).
PPT The Integumentary System PowerPoint Presentation, free download

Additional Medical Terms Integumentary System Medical Terminology
This page titled 14.1: Integumentary Assessment Introduction is shared under a CC BY-SA 4.0 license and was authored, remixed, and/or curated by Ernstmeyer & Christman (Eds.) via source content that was edited to the style and standards of the LibreTexts platform; a detailed edit history is available upon request.
Assessment of Integumentary Function
14.4 Integumentary Assessment Open Resources for Nursing (Open RN) Now that we have reviewed the anatomy of the integumentary system and common integumentary conditions, let's review the components of an integumentary assessment. The standard for documentation of skin assessment is within 24 hours of admission to inpatient care.
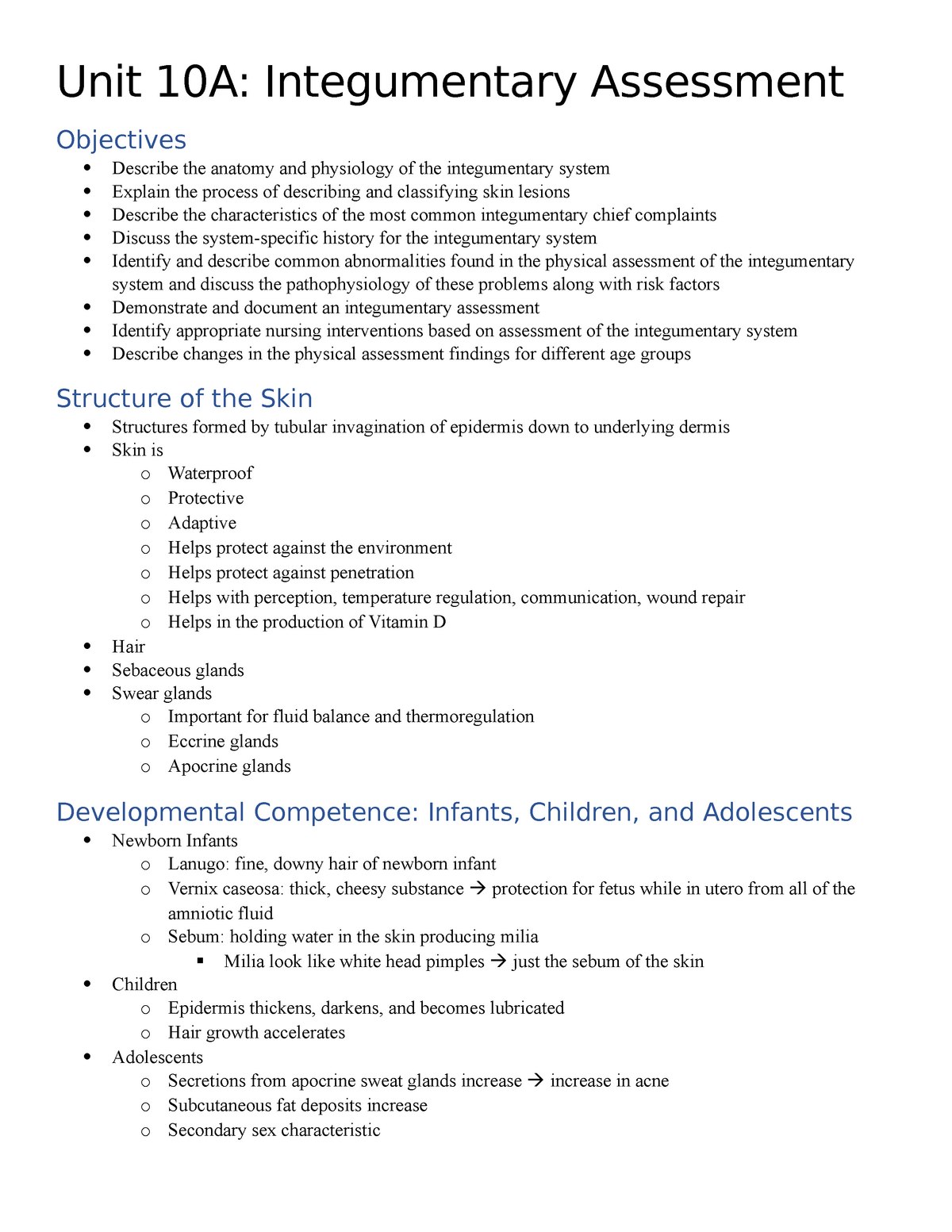
Unit 10A Notes Integumentary Assessment Unit 10A Integumentary
14.4 Integumentary Assessment Open Resources for Nursing (Open RN) Now that we have reviewed the anatomy of the integumentary system and common integumentary conditions, let's review the components of an integumentary assessment. The standard for documentation of skin assessment is within 24 hours of admission to inpatient care.
04 Integumentary System
14.3 Common Integumentary Conditions Now that we have reviewed the anatomy of the integumentary system, let's review common conditions that you may find during a routine integumentary assessment. Acne. Acne is a skin disturbance that typically occurs on areas of the skin that are rich in sebaceous glands, such as the face and back. It is most.
PPT Assessment of Clients with Integumentary Disorders PowerPoint
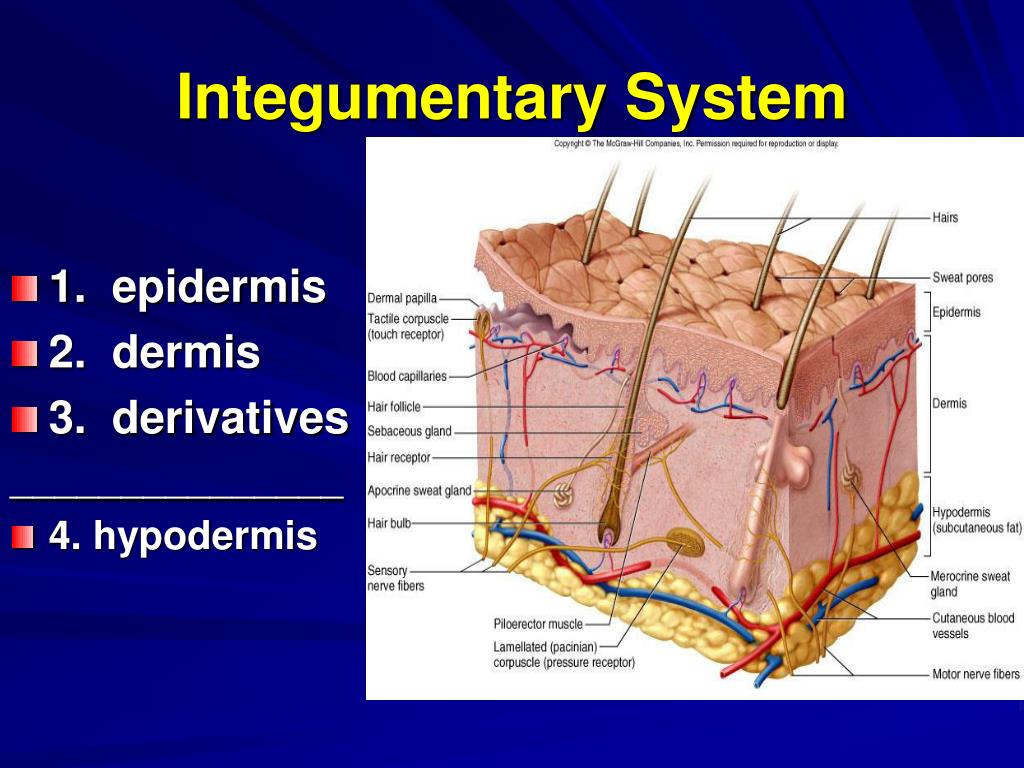
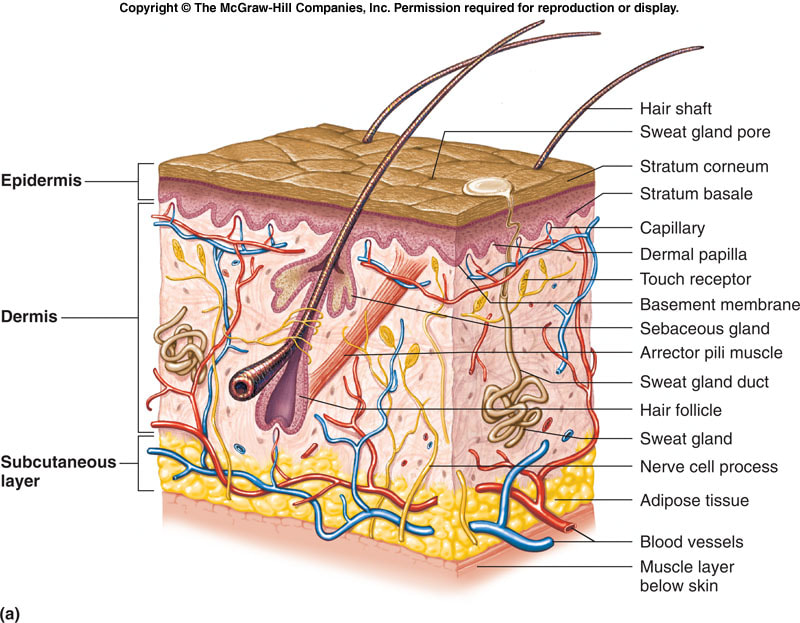
14.2 Basic Integumentary Concepts The integumentary system includes the skin, hair, and nails. The skin is an organ that performs a variety of essential functions, such as protecting the body from invasion by microorganisms, chemicals, and other environmental factors; preventing dehydration; acting as a sensory organ; modulating body temperature and electrolyte balance; and synthesizing.

Integumentary Handouts Nursing School Studying, Nursing School Notes
14.4 Integumentary Assessment. Open Resources for Nursing (Open RN) 14.5 Administering Intradermal Medications. Open Resources for Nursing (Open RN) 14.6 Sample Documentation. Open Resources for Nursing (Open RN) 14.7 Checklist for Integumentary Assessment.
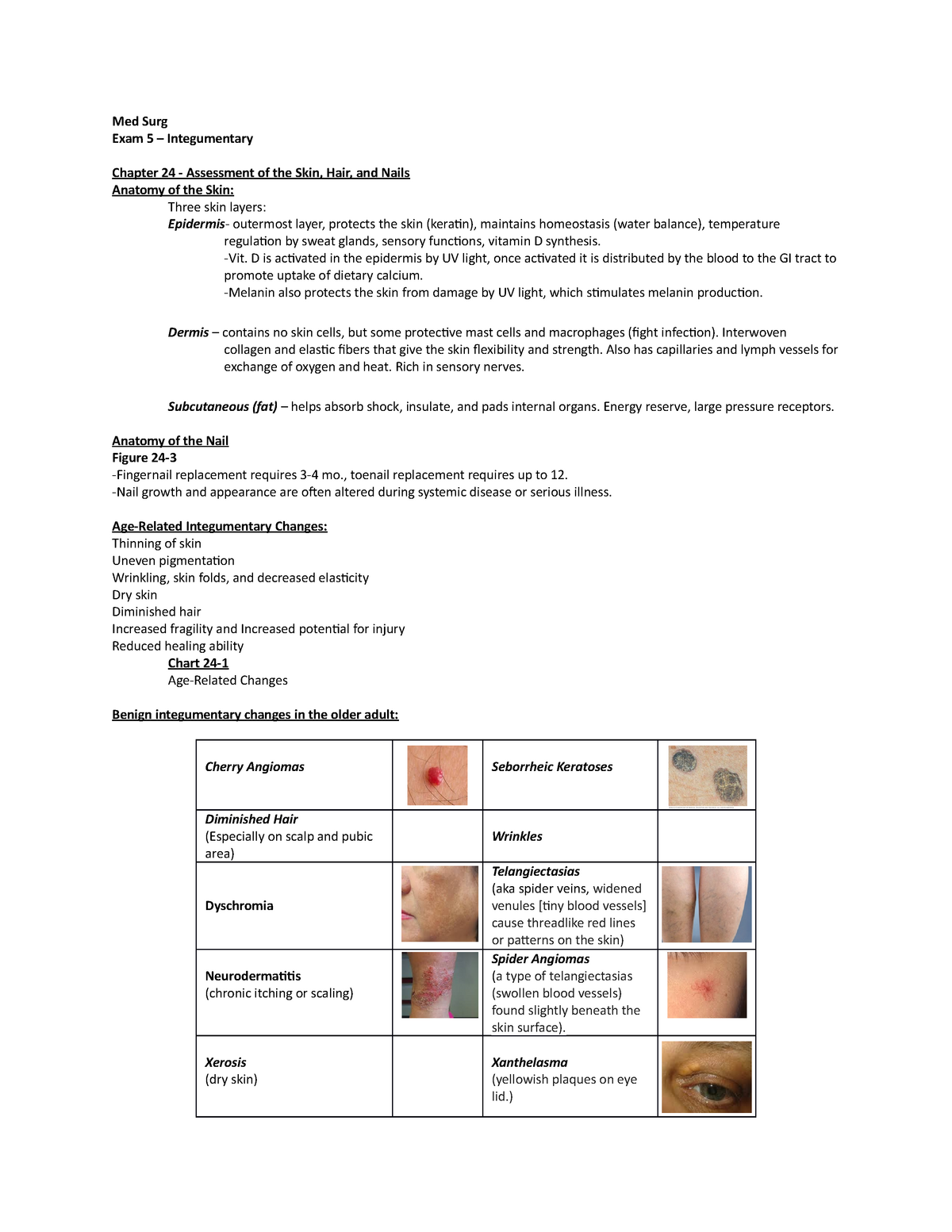
Integumentary Exam Med Surg Exam 5 Integumentary Chapter 24
See Figure 14.11 [8] for an illustration of the rule of nines. The head is 9% (4.5% on each side), the upper limbs are 9% each (4.5% on each side), the lower limbs are 18% each (9% on each side), and the trunk is 36% (18% on each side). Figure 14.11 Rule of Nines Scars. Most cuts and wounds cause scar formation.
Integumentary Systemanatomy,physiology, Common Problems, and
14.4. INTEGUMENTARY ASSESSMENT. Now that we have reviewed the anatomy of the integumentary system and common integumentary conditions, let's review the components of an integumentary assessment. The standard for documentation of skin assessment is within 24 hours of admission to inpatient care. Skin assessment should also be ongoing in.

Assessing The Integumentary System PDF Dermatitis Integumentary
Older adults may also be less able to sense touch, pressure, vibration, heat, and cold. [12] When completing an integumentary assessment it is important to distinguish between expected and unexpected assessment findings. Please review Table 14.4.2 14.4. 2 to review common expected and unexpected integumentary findings.

Checklist For Integumentary Assessment 1 PDF
Assessing the skin, hair, and nails is part of a routine head-to-toe assessment completed by registered nurses. During inpatient care, a comprehensive skin assessment on admission establishes a baseline for the condition of a patient's skin and is essential for developing a care plan for the prevention and treatment of skin injuries. [1] Before discussing the components of a routine skin.

14.4 Integumentary Assessment Nursing Skills 2e
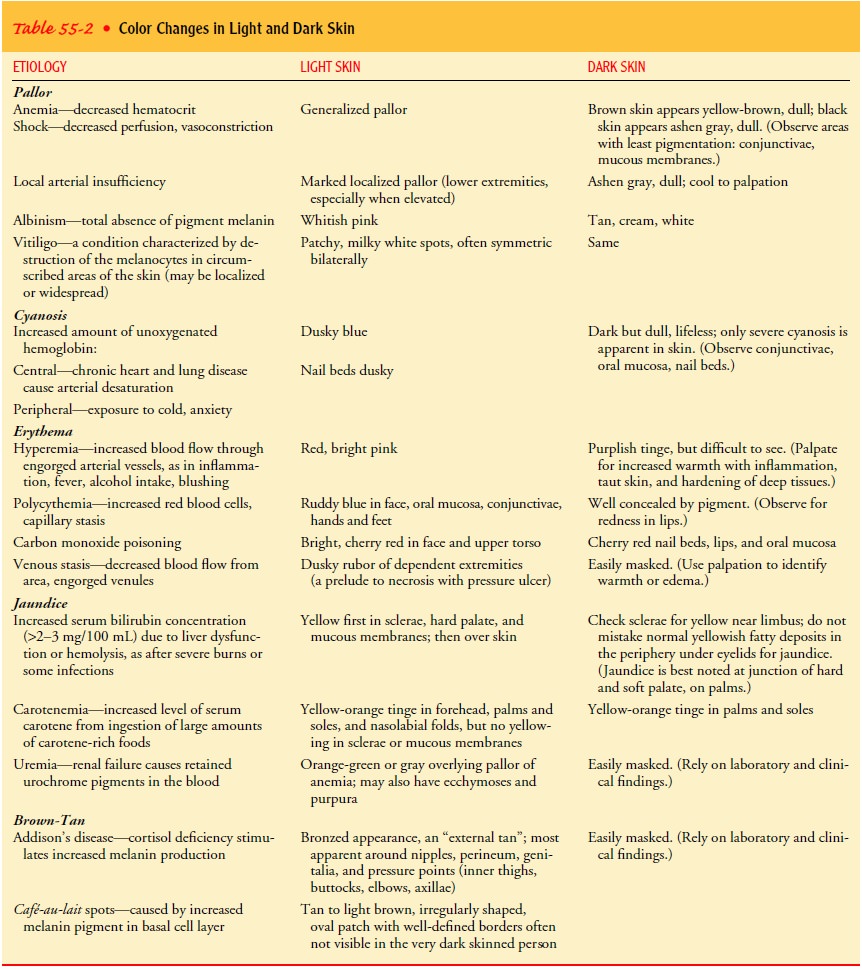
I. Overview of Assessment of the Integumentary System. The assessment of the integumentary system which includes the skin, hair and nails is an important element of the nurse's assessment of the patient's health status. These body structures do have specific functions but they also reflect functions or dysfunctions of other body systems as.

Medical Terminology of the Integumentary System Nursecepts (2022)
Learning Objectives. Perform an integumentary assessment including the skin, hair, and nails. Modify assessment techniques to reflect variations across the life span and ethnic and cultural variations. Assessing the skin, hair, and nails is part of a routine head-to-toe assessment completed by registered nurses.

SOLUTION Health assessment nursing integumentary assessment nursing
Introduction to Integumentary System The integumentary system includes the skin, hair,. As a nurse, it is important to hone your assessment skills and pay close attention to potential cues that may signal underlying concerns that require your intervention. See Figure 1 for an anatomical overview of the integumentary system.

Integumentary Assessment YouTube
How does the nurse document these assessment findings according to the muscle strength scale? 4 out of 5; 3 out of 5; 5 out of 5; 1 out of 5; 3. A young adult presents to the urgent care with a right knee injury. The injury occurred during a basketball game. The nurse begins to perform a musculoskeletal assessment. What is the first step of the.